Relief Is Here: New Guidelines for Menopause-Related Symptoms
Menopause is a natural transition, but many women are surprised by the physical symptoms that come with it. I’m not talking about the hot flashes and changes with menstruation - I’m talking about the symptoms that affect bladder and sexual function! Gone are the days of being brushed off by providers and being told to have a glass of wine. The American Urological Association (AUA) has just published their new 2025 guidelines for Genitourinary Syndrome of Menopause (link to full guidelines at bottom).
What is Genitourinary Syndrome of Menopause?
Genitourinary Syndrome of Menopause (GSM) describes a range of symptoms that arise due to the decline of estrogen and androgen levels in the genitourinary tract during menopause.(1)
Some very common symptoms you may experience include:
Pelvic pain
Pain with sexual activity (Dyspareunia)
Vaginal dryness
Bladder leakage
Urinary Urgency and Frequency
Difficulty achieving orgasm
Urinary Tract Infections (UTIs)
As hormone levels decline, the vulvovaginal tissue becomes more thin, frail, and loses moisture, which can lead to any of the symptoms listed above. Pelvic floor dysfunction is often accompanied by these changes and can perpetuate symptoms. It is estimated that between 13-87% of post-menopausal women experience GSM.(1)
8 Key Takeaways from the Guidelines
Patients should be screened for GSM for genital, sexual, and/or urinary symptoms using a focused medical, sexual, and psychosocial history.
In patients with GSM and pelvic floor dysfunction, clinicians may refer to a physical therapist specializing in pelvic floor conditions.
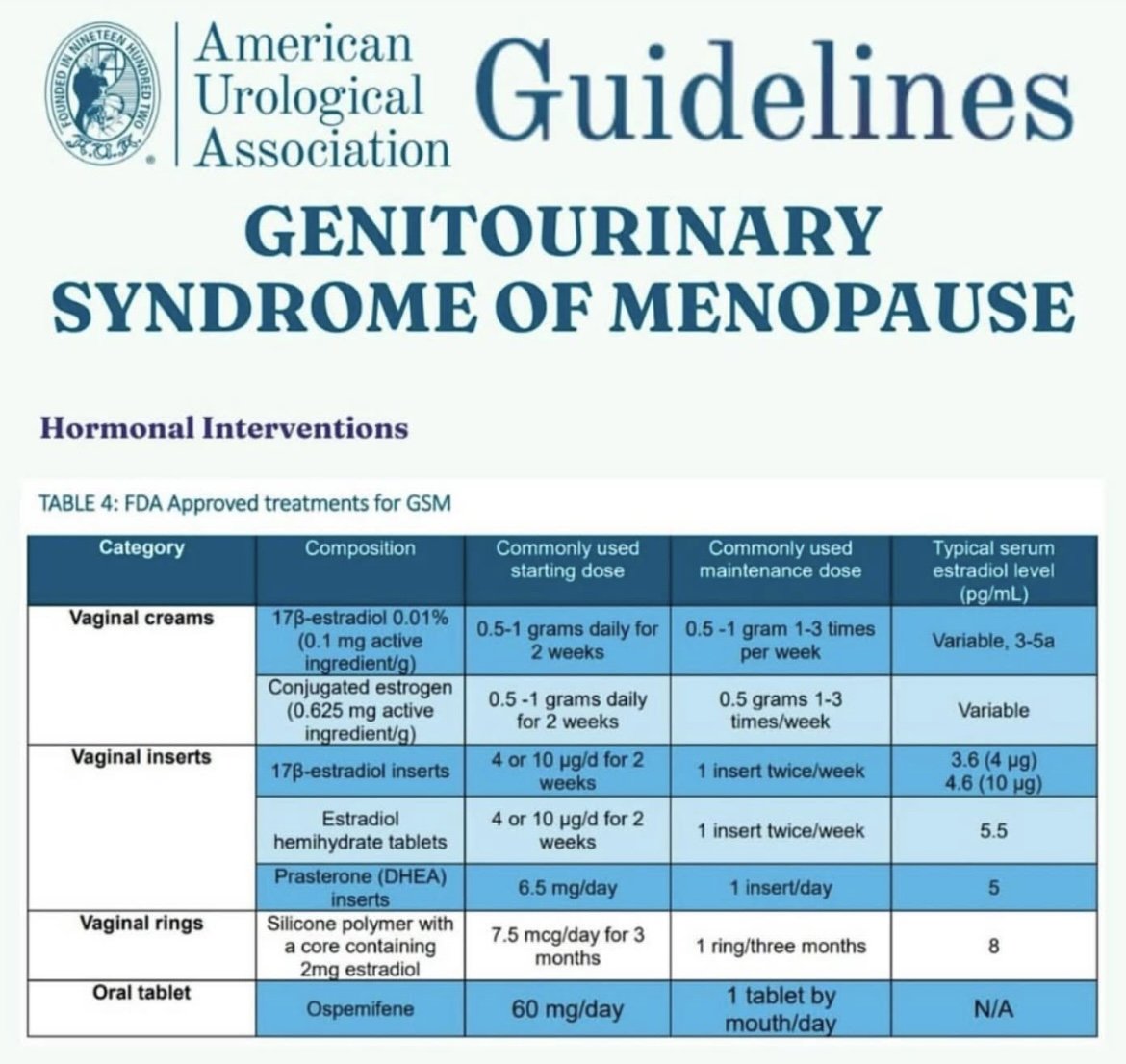
Clinicians should offer the option of local low-dose vaginal estrogen to patients with GSM to improve vulvovaginal discomfort/irritation, dryness, and/or dyspareunia.
Clinicians should offer the option of vaginal dehydroepiandrosterone (DHEA) to patients with GSM to improve vulvovaginal dryness and/or dyspareunia.
local low-dose vaginal estrogen, does not increase the risk for endometrial hyperplasia with atypia or endometrial cancer.
Clinicians should inform patients of the absence of evidence linking local low-dose vaginal estrogen to the development of breast cancer.
Neither vaginal dehydroepiandrosterone (DHEA) nor ospemifene increase the risk for breast cancer.
For patients with GSM who have a personal history of breast cancer, clinicians may recommend local low-dose vaginal estrogen in the context of multi-disciplinary shared decision-making.
Why This Matters
Many women have suffered in silence or have been told hormone treatment isn’t safe. These guidelines help reduce stigma and misinformation around hormone therapy, offering real options for relief! It also reinforces the value of pelvic floor therapy in managing these symptoms alongside hormonal treatment. When hormone treatment is in place, the tissue responds much quicker and easier to pelvic floor therapy.
What You Can Do
If you're experiencing any of the symptoms above, you don’t have to “just live with it.” Help is available. Pelvic floor therapy and updated medical treatment options can work together to restore your quality of life.
Give us a call today, to discuss how we can better help you and work alongside your physician for a collaborative approach to your menopause care!
I hope this information was helpful and maybe caused you to look at symptoms you have been ignoring. If you need help finding a pelvic floor therapist in Florida, we hope that you will consider us for either in-person or virtual appointments.
In the meantime, you can get more pelvic health content sent right to you, by completing the short form below👇