Your Radical Prostatectomy Recovery Guide
Understanding a Radial Prostatectomy
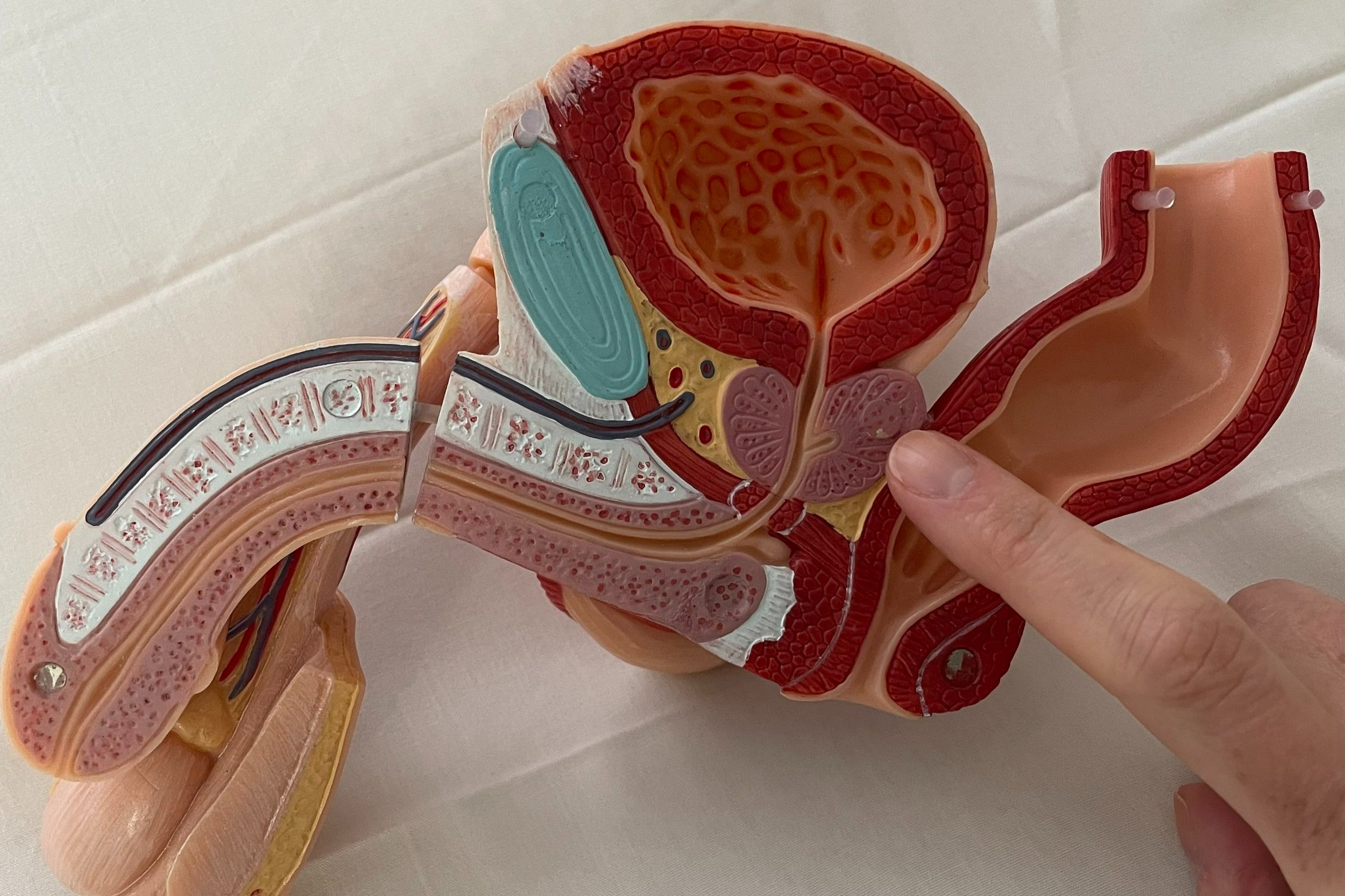
The prostate is a glad that sits just beneath the male bladder and surrounds the urethra (see image below). It functions to secrete fluid that makes up semen, in order to help carry sperm out of the urethra. As a side note, it is normal for a man’s prostate to become enlarged as he ages. This is known as Benign Prostatic Hyperplasia (BPH) and although it is non-cancerous, it can create unpleasant urinary symptoms on its own. BPH is not frequently treated with a prostatectomy.
According to the American Cancer Society, prostate cancer is the most common type of cancer among men over 50. A prostatectomy is a surgical procedure resulting in partial or complete removal of the prostate, typically due to prostate cancer. A radical prostatectomy is usually performed by making an incision above the pubic region but can also be done via laparoscopic incisions over the abdomen, or less frequently, through the perineum.
What to expect after surgery
Early On
Following a radical prostatectomy, you will have a temporary urinary catheter in place for 1-3 weeks. Once your physician removes the catheter, it can take some time for the urge to urinate to return. During the first few days following surgery, you’ll be encouraged to walk around at home but keep your activity level very light. Avoid prolonged bedrest and follow your post-op protocol from the hospital, to keep your incision(s) clean and dry.
Bladder Leakage After Prostatectomy
Bladder leakage is a very common side effect from surgery, that almost every man faces. The time it takes to resolve varies for each person but can be sped up with early intervention of pelvic floor therapy. You may experience any/all of the following for several weeks after surgery:
Dribbling after urination
Bladder leakage with the urge to urinate
Not making it to the toilet in time (urge incontinence)
Leakage with coughing/sneezing/laughing (stress incontinence)
Sexual Dysfunction After Prostatectomy
Difficulty achieving and maintaining erections is another very common complaint after surgery. In general, bladder control is regained before erections return. It can take 6-12 months to begin to see erections return. There is also the possibility that your surgeon may not be able to spare the nerves in this region, leading to incomplete return of erections or permanent loss of erections all together. This can create significant emotional distress but it’s important to manage expectations early on and have some patience during the rehab process. A percentage of patients also notice a decrease in penile length following surgery, which is another reason male pelvic floor therapy should be started soon after.
Pelvic floor therapy after surgery
Pelvic floor therapy following a radical prostatectomy is critical to your recovery! More and more physicians are automatically referring patients to therapy, as research shows this should be first line of treatment for recovery. How can pelvic floor therapy help after a prostatectomy?
Bladder retraining - To help establish optimal bladder habits in order to normalize functioning
Muscle retraining - A radical prostatectomy always involves disruption of the internal urethral sphincter, which is why bladder leakage is so common. Pelvic floor therapy helps you to optimize muscle coordination and strength at your pelvic floor, to compensate for the loss of this sphincter control. This allows you to get back to the activities you love without leakage.
Penile rehab - It is important to maintain blood flow and oxygen to the penile tissue after surgery, both for sexual function and to attempt to minimize length loss that some (but not all) men report. Pelvic floor therapists can guild you on using a penile pump to rehab the penis as well as erection rings to support an erection for sexual activity.
The importance of prehab
Seeing a pelvic floor therapist before your prostatectomy can greatly help you prepare for what to expect afterwards. Physicians don’t typically have the time to discuss in depth your toileting habits, sexual function, and review with you how to control your pelvic floor muscles. We cover all of this and more during your pre-surgical appointment(s). This can also give you peace of mind, knowing you have a medical team helping you through this difficult time. We don’t always see surgeons suggesting a pre-operative pelvic floor visit, so knowing how this can help you is important to be able to advocate for yourself!
What you can do next
If you’re considering a radical prostatectomy, or have one planned, get lined up with a pelvic floor therapist to guide you through the rehab (and prehab). If you’re local to Florida, we provide pelvic floor therapy for men, both in-person and virtually.
Here, you can download our 🔗Healing from your radical prostatectomy handout🔗for more information and tips.
Follow us on social media and sign up for our monthly newsletter below, for more pelvic health content.